Abstract
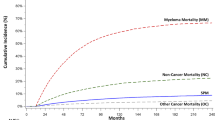
Solid organ transplant recipients have elevated cancer risks, owing in part to pharmacologic immunosuppression. However, little is known about risks for hematologic malignancies of myeloid origin. We linked the US Scientific Registry of Transplant Recipients with 15 population-based cancer registries to ascertain cancer occurrence among 207 859 solid organ transplants (1987–2009). Solid organ transplant recipients had a significantly elevated risk for myeloid neoplasms, with standardized incidence ratios (SIRs) of 4.6 (95% confidence interval 3.8–5.6; N=101) for myelodysplastic syndromes (MDS), 2.7 (2.2–3.2; N=125) for acute myeloid leukemia (AML), 2.3 (1.6–3.2; N=36) for chronic myeloid leukemia and 7.2 (5.4–9.3; N=57) for polycythemia vera. SIRs were highest among younger individuals and varied by time since transplantation and organ type (Poisson regression P<0.05 for all comparisons). Azathioprine for initial maintenance immunosuppression increased risk for MDS (P=0.0002) and AML (2–5 years after transplantation, P=0.0163). Overall survival following AML/MDS among transplant recipients was inferior to that of similar patients reported to US cancer registries (log-rank P<0.0001). Our novel finding of increased risks for specific myeloid neoplasms after solid organ transplantation supports a role for immune dysfunction in myeloid neoplasm etiology. The increased risks and inferior survival should heighten clinician awareness of myeloid neoplasms during follow-up of transplant recipients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Annual Data Report of the US Organ. Procurement and Transplantation Network (OPTN) and the Scientific Registry of Transplant Recipients (SRTR). Am J Transplant 2013; 13 (Suppl 1): 1–234.
Engels EA, Pfeiffer RM, Fraumeni JF, Kasiske BL, Israni AK, Snyder JJ et al. Spectrum of cancer risk among US solid organ transplant recipients. JAMA 2011; 306: 1891–1901.
Grulich AE, van Leeuwen MT . Falster MO, Vajdic CM. Incidence of cancers in people with HIV/AIDS compared with immunosuppressed transplant recipients: a meta-analysis. Lancet 2007; 370: 59–67.
Adami J, Gabel H, Lindelof B, Ekstrom K, Rydh B, Glimelius B et al. Cancer risk following organ transplantation: a nationwide cohort study in Sweden. Br J Cancer 2003; 89: 1221–1227.
Quinlan SC, Morton LM, Pfeiffer RM, Anderson LA, Landgren O, Warren JL et al. Increased risk for lymphoid and myeloid neoplasms in elderly solid-organ transplant recipients. Cancer Epidemiol Biomarkers Prev 2010; 19: 1229–1237.
Offman J, Opelz G, Doehler B, Cummins D, Halil O, Banner NR et al. Defective DNA mismatch repair in acute myeloid leukemia/myelodysplastic syndrome after organ transplantation. Blood 2004; 104: 822–828.
Gale RP, Opelz G . Commentary: does immune suppression increase risk of developing acute myeloid leukemia? Leukemia 2012; 26: 422–423.
Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H et al. World Health Organization Classification of Tumours of Haematopoietic and Lymphoid Tissues. IARC Press: Lyon, 2008.
Howlader N, Noone A, Krapcho M, Garshell J, Neyman N, Altekruse S et al. SEER Cancer Statistics Review, 1975-2010, National Cancer Institute. Bethesda, MD, USA 2013.
Leone G, Fianchi L, Pagano L, Voso MT . Incidence and susceptibility to therapy-related myeloid neoplasms. Chem Biol Interact 2010; 184: 39–45.
Anderson LA, Duncombe AS, Hughes M, Mills ME, Wilson JC, McMullin MF . Environmental, lifestyle, and familial/ethnic factors associated with myeloproliferative neoplasms. Am J Hematol 2012; 87: 175–182.
Anderson LA, Pfeiffer RM, Landgren O, Gadalla S, Berndt SI, Engels EA . Risks of myeloid malignancies in patients with autoimmune conditions. Br J Cancer 2009; 100: 822–828.
Kristinsson SY, Landgren O, Samuelsson J, Bjorkholm M, Goldin LR . Autoimmunity and the risk of myeloproliferative neoplasms. Haematologica 2010; 95: 1216–1220.
Kristinsson SY, Bjorkholm M, Hultcrantz M, Derolf AR, Landgren O, Goldin LR . Chronic immune stimulation might act as a trigger for the development of acute myeloid leukemia or myelodysplastic syndromes. J Clin Oncol 2011; 29: 2897–2903.
Ramadan SM, Fouad TM, Summa V, Hasan S, Lo-Coco F . Acute myeloid leukemia developing in patients with autoimmune diseases. Haematologica 2012; 97: 805–817.
Frisch M, Biggar RJ, Engels EA, Goedert JJ, AIDS-Cancer Match Registry Study Group. Association of cancer with AIDS-related immunosuppression in adults. JAMA 2001; 285: 1736–1745.
Shiels MS, Engels EA . Increased risk of histologically defined cancer subtypes in human immunodeficiency virus-infected individuals: clues for possible immunosuppression-related or infectious etiology. Cancer 2012; 118: 4869–4876.
Fritz AG . International classification of diseases for oncology (ICD-O) 3rd edn World Health Organization: Geneva, 2000.
van Leeuwen MT, Grulich AE, Webster AC, McCredie MRE, Stewart JH, McDonald SP et al. Immunosuppression and other risk factors for early and late non-Hodgkin lymphoma after kidney transplantation. Blood 2009; 114: 630–637.
Clarke CA, Morton LM, Lynch C, Pfeiffer RM, Hall EC, Gibson TM et al. Risk of lymphoma subtypes after solid organ transplantation in the United States. Br J Cancer 2013; 109: 280–288.
Quinlan SC, Pfeiffer RM, Morton LM, Engels EA . Risk factors for early-onset and late-onset post-transplant lymphoproliferative disorder in kidney recipients in the United States. Am J Hematol 2011; 86: 206–209.
Ghobrial IM, Habermann TM, Macon WR, Ristow KM, Larson TS, Walker RC et al. Differences between early and late posttransplant lymphoproliferative disorders in solid organ transplant patients: are they two different diseases? Transplantation 2005; 79: 244–247.
Bo J, Schroder H, Kristinsson J, Madsen B, Szumlanski C, Weinshilboum R et al. Possible carcinogenic effect of 6-mercaptopurine on bone marrow stem cells: relation to thiopurine metabolism. Cancer 1999; 86: 1080–1086.
Relling MV, Yanishevski Y, Nemec J, Evans WE, Boyett JM, Behm FG et al. Etoposide and antimetabolite pharmacology in patients who develop secondary acute myeloid leukemia. Leukemia 1998; 12: 346–352.
Smith SM . Clinical-cytogenetic associations in 306 patients with therapy-related myelodysplasia and myeloid leukemia: the University of Chicago series. Blood 2003; 102: 43–52.
Kwong Y-L . Azathioprine: association with therapy-related myelodysplastic syndrome and acute myeloid leukemia. J Rheumatol 2010 2010; 37: 485–490.
Knipp S, Hildebrandt B, Richter J, Haas R, Germing U, Gattermann N . Secondary myelodysplastic syndromes following treatment with azathioprine are associated with aberrations of chromosome 7. Haematologica 2005; 90: 691–693.
Putzki N, Knipp S, Ramczykowski T, Vago S, Germing U, Diener HC et al. Secondary myelodysplastic syndrome following long-term treatment with azathioprine in patients with multiple sclerosis. Mult Scler 2006; 12: 363–366.
Karran P, Attard N . Thiopurines in current medical practice: molecular mechanisms and contributions to therapy-related cancer. Nat Rev Cancer 2008; 8: 24–36.
Dickinson DM, Bryant PC, Williams MC, Levine GN, Li S, Welch JC et al. Transplant data: sources, collection, and caveats. Am J Transplant 2004; 4 (Suppl 9): 13–26.
Dutka P . Erythropoiesis-stimulating agents for the management of anemia of chronic kidney disease: past advancements and current innovations. Nephrol Nurs J 2012; 39: 447–457.
Ulrich F, Pratschke J, Neumann U, Pascher A, Puhl G, Fellmer P et al. Eighteen years of liver transplantation experience in patients with advanced Budd-Chiari syndrome. Liver Transpl 2008; 14: 144–150.
Langabeer SE, Burke A, McCarron SL, Kelly J, Carroll P, Browne PV et al. Chronic myeloid leukaemia presenting post-radiotherapy for prostate cancer: further evidence for an immunosurveillance effect. Br J Haematol 2013; 162: 708–710.
Wu SP, Costello R, Hofmann JN, Korde N, Mailankody S, Purdue M et al. MGUS prevalence in a cohort of AML patients. Blood 2013; 122: 294–295.
Engels EA, Preiksaitis J, Zingone A, Landgren O . Circulating antibody free light chains and risk of posttransplant lymphoproliferative disorder. Am J Transplant 2012; 12: 1268–1274.
Landgren O, Goedert JJ, Rabkin CS, Wilson WH, Dunleavy K, Kyle RA et al. Circulating serum free light chains as predictive markers of AIDS-related lymphoma. J Clin Oncol 2010; 28: 773–779.
Acknowledgements
This research was supported in part by the Intramural Program of the National Cancer Institute, National Institutes of Health and the Surveillance, Epidemiology and End Results Program. We gratefully acknowledge the support and assistance provided by individuals at the Health Resources and Services Administration (Monica Lin), the SRTR (Ajay Israni, Bertram Kasiske, Paul Newkirk and Jon Snyder) and the following cancer registries: the states of California, Colorado (Jack Finch), Connecticut (Lou Gonsalves), Georgia (Rana Bayakly), Hawaii (Brenda Hernandez), Iowa, Illinois (Lori Koch), Michigan (Glenn Copeland), New Jersey (Xiaoling Niu), New York (Amy Kahn), North Carolina (Chandrika Rao), Texas (Melanie Williams) and Utah (Janna Harrell), and the Seattle-Puget Sound area of Washington (Margaret Madeleine). We also thank analysts at Information Management Services for programming support (David Castenson, Matthew Chaloux, Michael Curry and Ruth Parsons). The views expressed in this paper are those of the authors and should not be interpreted to reflect the views or policies of the National Cancer Institute, Health Resources and Services Administration, SRTR, cancer registries or their contractors. This research was supported in part by the Intramural Research Program of the National Cancer Institute. During the initial period when registry linkages were performed, the SRTR was managed by Arbor Research Collaborative for Health in Ann Arbor, MI (contract HHSH234200537009C); beginning in September 2010, the SRTR was managed by Minneapolis Medical Research Foundation in Minneapolis, MN (HHSH250201000018C). The following cancer registries were supported by the National Program of Cancer Registries of the Centers for Disease Control and Prevention: California (agreement 1U58 DP000807-01), Colorado (U58 DP000848-04), Georgia (5U58DP000817-05), Illinois (5658DP000805-04), Michigan (5U58DP000812-03), New Jersey (5U58/DP000808-05), New York (U58DP0038789), North Carolina (U58DP000832) and Texas (5U58DP000824-04). The following cancer registries were supported by the SEER Program of the National Cancer Institute: California (contracts HHSN261201000036C, HHSN261201000035C and HHSN261201000034C), Connecticut (HHSN261201000024C), Hawaii (HHSN261201000037C, N01-PC-35137 and N01-PC-35139), Iowa (HSN261201000032C and N01-PC-35143), New Jersey (HHSN261201000027C and N01-PC-54405), Seattle-Puget Sound (N01-PC-35142) and Utah (HHSN261201000026C). Additional support was provided by the states of California, Colorado, Connecticut, Illinois, Iowa, New Jersey, New York (Cancer Surveillance Improvement Initiative 14-2491), Texas and Washington, as well as the Fred Hutchinson Cancer Research Center in Seattle, WA.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Author contributions
LMM, TMG and EAE designed the research; CAC, CFL and EAE collected data; LMM, TMG and EAE analyzed the data; all authors interpreted data and made critical contributions to the manuscript; LMM wrote the manuscript.
Supplementary Information accompanies this paper on the Leukemia website
Supplementary information
Rights and permissions
About this article
Cite this article
Morton, L., Gibson, T., Clarke, C. et al. Risk of myeloid neoplasms after solid organ transplantation. Leukemia 28, 2317–2323 (2014). https://doi.org/10.1038/leu.2014.132
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2014.132
This article is cited by
-
Myelodysplastic syndromes
Nature Reviews Disease Primers (2022)
-
Therapy-related myeloid neoplasms with different latencies: a detailed clinicopathologic analysis
Modern Pathology (2022)
-
Chronic myeloid leukemia in solid organ transplant patients: a case series
International Journal of Hematology (2021)
-
Allogeneic hematopoietic stem cell transplantation in a prior lung transplant recipient
International Journal of Hematology (2020)
-
An emerging trend of rapid increase of leukemia but not all cancers in the aging population in the United States
Scientific Reports (2019)