Abstract
Background and Objectives
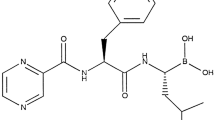
The proteasome inhibitor bortezomib is approved for the treatment of multiple myeloma (MM) and, in the US, for the treatment of mantle cell lymphoma following at least one prior therapy; the recommended dose and schedule is 1.3 mg/m2 on days 1, 4, 8 and 11 of 21-day cycles, and the approved routes of administration in the US prescribing information are by intravenous and, following a recent update, subcutaneous injection. Findings from a phase III study demonstrated that subcutaneous administration of bortezomib, using the same dose and schedule, resulted in similar efficacy with an improved systemic safety profile (including significantly lower rates of peripheral neuropathy) versus intravenous bortezomib in patients with relapsed MM. The objectives of this report were to present a comprehensive analysis of the pharmacokinetics and pharmacodynamics of subcutaneous versus intravenous bortezomib, and to evaluate the impact of the subcutaneous administration site, subcutaneous injection concentration and demographic characteristics on bortezomib pharmacokinetics and pharmacodynamics.
Patients and Methods
Data were analysed from the pharmacokinetic substudy of the randomized phase III MMY-3021 study and the phase I CAN-1004 study of subcutaneous versus intravenous bortezomib in patients aged ≥18 (MMY-3021) or ≤75 (CAN-1004) years with symptomatic relapsed or refractory MM after 1–3 (MMY-3021) or ≥1 (CAN-1004) prior therapies. Patients received up to eight 21-day cycles of subcutaneous or intravenous bortezomib 1.3 mg/m2 on days 1, 4, 8 and 11. Pharmacokinetic and pharmacodynamic (20S proteasome inhibition) parameters of bortezomib following subcutaneous or intravenous administration were evaluated on day 11, cycle 1.
Results
Bortezomib systemic exposure was equivalent with subcutaneous versus intravenous administration in MMY-3021 [mean area under the plasma concentration–time curve from time zero to the last quantifiable timepoint (AUClast): 155 vs. 151 ng·h/mL; geometric mean ratio 0.992 (90 % CI 80.18, 122.80)] and comparable in CAN-1004 (mean AUClast: 195 vs. 241 ng·h/mL); maximum (peak) plasma drug concentration (Cmax) was lower with subcutaneous administration in both MMY-3021 (mean 20.4 vs. 223 ng/mL) and CAN-1004 (mean 22.5 vs. 162 ng/mL), and time to Cmax (tmax) was longer with subcutaneous administration in both studies (median 30 vs. 2 min). Blood 20S proteasome inhibition pharmacodynamic parameters were also similar with subcutaneous versus intravenous bortezomib: mean maximum effect (Emax) was 63.7 versus 69.3 % in MMY-3021 and 57.0 versus 68.8 % in CAN-1004, and mean area under the effect–time curve from time zero to 72 h was 1,714 versus 1,383 %·h in MMY-3021 and 1,619 versus 1,283 %·h in CAN-1004. Time to Emax was longer with subcutaneous administration in MMY-3021 (median 120 vs. 5 min) and CAN-1004 (median 120 vs. 3 min). Concentration of the subcutaneous injected solution had no appreciable effect on pharmacokinetic or pharmacodynamic parameters. There were no apparent differences in bortezomib pharmacokinetic and pharmacodynamic parameters between subcutaneous administration in the thigh or abdomen. There were also no apparent differences in bortezomib exposure related to body mass index, body surface area or age.
Conclusion
Subcutaneous administration results in equivalent bortezomib plasma exposure to intravenous administration, together with comparable blood 20S proteasome inhibition pharmacodynamic effects. These findings, together with the non-inferior efficacy of subcutaneous versus intravenous bortezomib demonstrated in MMY-3021, support the use of bortezomib via the subcutaneous route across the settings of clinical use in which the safety and efficacy of intravenous bortezomib has been established.




Similar content being viewed by others
References
Janssen-Cilag International N.V. VELCADE® (bortezomib): summary of product characteristics. Beerse: Janssen-Cilag International N.V.; 2009.
Millennium Pharmaceuticals Inc. VELCADE® (bortezomib) for injection: prescribing information. Rev. 13. Cambridge: Millennium Pharmaceuticals Inc.; 2012.
Moreau P, Pylypenko H, Grosicki S, Karamanesht I, Leleu X, Grishunina M, et al. Subcutaneous versus intravenous administration of bortezomib in patients with relapsed multiple myeloma: a randomised, phase 3, non-inferiority study. Lancet Oncol. 2011;12:431–40.
Moreau P, Coiteux V, Hulin C, Leleu X, van de Velde H, Acharya M, et al. Prospective comparison of subcutaneous versus intravenous administration of bortezomib in patients with multiple myeloma. Haematologica. 2008;93:1908–11.
Greipp PR, San MJ, Durie BG, Crowley JJ, Barlogie B, Blade J, et al. International staging system for multiple myeloma. J Clin Oncol. 2005;23:3412–20.
Lightcap ES, McCormack TA, Pien CS, Chau V, Adams J, Elliott PJ. Proteasome inhibition measurements: clinical application. Clin Chem. 2000;46:673–83.
Lundin J, Kimby E, Bjorkholm M, Broliden PA, Celsing F, Hjalmar V, et al. Phase II trial of subcutaneous anti-CD52 monoclonal antibody alemtuzumab (Campath-1H) as first-line treatment for patients with B-cell chronic lymphocytic leukemia (B-CLL). Blood. 2002;100:768–73.
Quinn DI, Nemunaitis J, Fuloria J, Britten CD, Gabrail N, Yee L, et al. Effect of the cytochrome P450 2C19 inhibitor omeprazole on the pharmacokinetics and safety profile of bortezomib in patients with advanced solid tumours, non-Hodgkin’s lymphoma or multiple myeloma. Clin Pharmacokinet. 2009;48:199–209.
Venkatakrishnan K, Rader M, Ramanathan RK, Ramalingam S, Chen E, Riordan W, et al. Effect of the CYP3A inhibitor ketoconazole on the pharmacokinetics and pharmacodynamics of bortezomib in patients with advanced solid tumors: a prospective, multicenter, open-label, randomized, two-way crossover drug–drug interaction study. Clin Ther. 2009;31(Pt 2):2444–58.
Hellmann A, Rule S, Walewski J, Shpilberg O, Feng H, van de Velde H, et al. Effect of cytochrome P450 3A4 inducers on the pharmacokinetic, pharmacodynamic and safety profiles of bortezomib in patients with multiple myeloma or non-Hodgkin’s lymphoma. Clin Pharmacokinet. 2011;50:781–91.
Leal TB, Remick SC, Takimoto CH, Ramanathan RK, Davies A, Egorin MJ, et al. Dose-escalating and pharmacological study of bortezomib in adult cancer patients with impaired renal function: a National Cancer Institute Organ Dysfunction Working Group Study. Cancer Chemother Pharmacol. 2011;68:1439–47.
LoRusso PM, Venkatakrishnan K, Ramanathan RK, Sarantopoulos J, Mulkerin D, Shibata SI, et al. Pharmacokinetics and safety of bortezomib in patients with advanced malignancies and varying degrees of liver dysfunction: phase I NCI Organ Dysfunction Working Group Study NCI-6432. Clin Cancer Res. 2012;18:2954–63.
Acknowledgments
These studies were funded by Janssen Research & Development (formerly Johnson & Johnson Pharmaceutical Research & Development, L.L.C.) and Millennium Pharmaceuticals, Inc. Representatives of the sponsors were involved in the study design, data collection, data analysis, data interpretation, and writing and reviewing of the manuscript, as indicated by their inclusion as co-authors. The corresponding author had full access to all data in the studies and had final responsibility for the decision to submit for publication. The authors would like to acknowledge the writing assistance of Steve Hill of FireKite in the development of this manuscript, which was funded by Millennium Pharmaceuticals, Inc., and Janssen Global Services.
Conflicts of interest
P.M.: advisory board membership, honoraria, Janssen and Millennium Pharmaceuticals, Inc.; I.I.K.: no conflicts of interest; N.D.: no conflicts of interest; M.Y.K.: no conflicts of interest; K.V.V.: no conflicts of interest; V.A.D.: no conflicts of interest; A.S.: no conflicts of interest; C.H.: honoraria, Janssen-Cilag, Celgene; X.L.: institutional grants, lecture fees, Janssen; D.-L.E.: employment, Millennium Pharmaceuticals, Inc., stock ownership, Johnson & Johnson; K.V.: employment, Millennium Pharmaceuticals, Inc.; D.S.: employment, Janssen R&D; H.F.: employment, Janssen R&D; S.G.: employment, Janssen R&D, stock ownership, Johnson & Johnson; A.C.: employment, Janssen R&D; H.vdV.: employment, Janssen R&D, stock ownership, Johnson & Johnson; W.D.: employment, Janssen R&D, stock ownership, Johnson & Johnson; T.F.: speakers bureau, advisory committee, Janssen.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Moreau, P., Karamanesht, I.I., Domnikova, N. et al. Pharmacokinetic, Pharmacodynamic and Covariate Analysis of Subcutaneous Versus Intravenous Administration of Bortezomib in Patients with Relapsed Multiple Myeloma. Clin Pharmacokinet 51, 823–829 (2012). https://doi.org/10.1007/s40262-012-0010-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-012-0010-0