Abstract
Introduction
We evaluated incidence, prevalence, costs, and healthcare utilization associated with systemic lupus erythematosus (SLE) in patients in Germany.
Methods
Adult patients with SLE were identified from the German Betriebskrankenkassen (BKK) health insurance fund database between 2009 and 2014. SLE incidence and prevalence were calculated for each year and extrapolated (age and sex adjusted) to the German population. The 2009 SLE population was followed through 2014. Healthcare utilization and costs for patients with SLE were calculated and compared with controls matched by age, sex, and baseline Charlson Comorbidity Index scores.
Results
This analysis included 1160 patients with SLE. Estimated SLE incidence between 2009 and 2014 ranged from 4.59 to 6.89 per 100,000 persons and prevalence ranged from 37.32 to 47.36 per 100,000. SLE incidence in Germany in 2014 was 8.82 per 100,000 persons; prevalence was 55.80 (corrected for right-censored data). At baseline, 12.8, 41.7, and 45.5% of patients were categorized as having mild, moderate, and severe SLE, respectively. Patients with SLE had greater mean (standard deviation [SD]) annual medical costs compared with matched controls 1 year after index diagnosis (€6895 [14,424] vs. €3692 [3994]; P < 0.0001) and in subsequent years. Patients with moderate or severe SLE had significantly more hospitalizations, outpatient visits, and prescription medication use compared with matched controls. Mean annual costs for 5 years ranged from €1890 to 3010, €4867 to 5876, and €8396 to 10,001 for patients with mild, moderate, and severe SLE, respectively.
Conclusions
SLE incidence in Germany increased 1.4-fold over 5 years. Patients with SLE have higher healthcare costs, and costs increase with baseline severity. Early and effective treatments may delay progression and reduce the burden of SLE.
Similar content being viewed by others
Why carry out this study? |
The burden of systemic lupus erythematosus (SLE) continues to evolve, and although current SLE therapies may modify the disease course, alleviate symptoms, and improve short- to medium-term survival, patients with SLE continue to have sustained disease activity, accrue organ damage, and experience decreased quality of life. |
There are limited data on long-term SLE studies that describe how disease severity may affect healthcare resource utilization and work disability over time globally, including in Germany, where current SLE incidence and prevalence estimates are also limited. |
We used claims data from a German health insurance fund database from 2009 to 2014 to assess trends in SLE incidence and prevalence, treatment patterns, and the role of disease severity on healthcare resource utilization and costs for patients with SLE in Germany. |
What was learned from the study? |
The incidence of SLE in Germany is increasing, with the 2014 SLE incidence of 8.82 per 100,000 persons representing a 1.4-fold increase over 2009. |
SLE healthcare resource utilization and costs are also increasing compared with age-, sex-, and comorbidity-matched controls, and disease severity (moderate and severe SLE), is an important driver of healthcare resource utilization and costs. |
The rising SLE incidence and prevalence, and associations between disease severity and costs, highlight the need for timely diagnosis, early treatment, and new therapies to prevent or delay disease progression, thereby reducing the burden of SLE. |
Digital Features
This article is published with digital features, including a summary slide, to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.13526234.
Introduction
Systemic lupus erythematosus (SLE) is a complex chronic inflammatory autoimmune disorder that involves several organ systems, including mucocutaneous, musculoskeletal, hematopoietic, cardiovascular, respiratory, renal, and nervous systems [1]. SLE is associated with a threefold increase in mortality, with the leading causes being cardiovascular disease, severe renal dysfunction, and infection [2]. The 5-year survival rates for SLE generally increased from the 1950s to the 1990s, and then plateaued at 93−95% [3]. In a meta-analysis, the 10-year survival estimates between 2008 and 2016 were 89% and 85% for adults with SLE from high- and low-/middle-income countries, respectively [4].
There is no cure for SLE; however, current therapies help modify the disease course, alleviate symptoms, and improve survival [1, 5, 6]. Despite an increase in short- to medium-term survival, [4] patients with SLE continue to incur organ involvement, accrue organ damage, and experience decreased quality of life [7], indicating an unmet need for novel therapies.
It is important to establish how SLE disease progression affects healthcare resource utilization and work disability over time in many countries, including Germany. Longer-term SLE studies with patient segmentation by disease severity and subcategorization of costs will improve the characterization of the burden of SLE [8].
In this retrospective observational cohort study, we assessed the burden of illness, treatment patterns, and the effect of disease activity on healthcare resource utilization and costs for patients with SLE in Germany. We utilized data of statutorily insured patients in Germany from the Betriebskrankenkassen (BKK) health insurance fund database to estimate annual SLE incidence and prevalence in the German population from 2009 to 2014. Diagnoses of patients identified with SLE in 2009 were validated. Patients were stratified by disease severity and evaluated over 5 years to assess disease progression and healthcare resource utilization.
Methods
BKK Health Insurance Data
We used anonymized claims data from 2009 to 2014 from a German BKK health insurance fund database of 4.14 million insured persons. The BKK health insurance fund is one of six branches of the statutory health insurance in Germany; it is the category most representative of persons insured across all branches of German statutory health insurance [9]. These data link ambulatory and hospital care settings and describe medical care, including hospitalizations, sick leave, and mortality of the German population insured via statutory health insurance (GKV population). Approximately 87% of the German population is insured primarily with this statutory insurance, and such insurance is mandatory for employees earning below a defined income threshold [10]. Patient care is assessed according to German Procedure Classification codes, German Diagnosis Related Groups codes, and International Classification of Diseases, 10th Revision (ICD-10) diagnosis codes (Supplementary Table S1).
Health insurance companies were informed about the project, and required approvals were obtained. Patient-level data in the database are anonymized to comply with German data protection regulations. Use of this database for health services research is fully compliant with German federal law, and accordingly, Institutional Review Board/ethical approval was not required because all patient-level data in the database are anonymized. The study conformed with the Helsinki Declaration of 1964, as revised in 2013, concerning human and animal rights. Springer’s policy concerning informed consent does not apply to this analysis of de-identified claims data. To evaluate how well the BKK sample represents the German population, age and sex of the BKK sample in 2009 were compared with that of 70.0 million persons in the GKV population.
Study Sample
Eligible patients were insured and documented in the database between 2009 and 2014 with a confirmed or reliable ICD-10 SLE diagnosis (M32.1 [SLE with organ or system involvement], M32.8 [other forms of SLE], and M32.9 [SLE, unspecified]) [11]. Patients younger than 18 years, with missing data, or with drug-induced SLE (code M32.0) were excluded. We required patients to be insured and included in the database for at least 3 years before study entry (baseline) to differentiate incident from prevalent SLE (Fig. 1a). Baseline characteristics were identified in the time frame from the earliest study quarter with SLE diagnosis (which coincided with the index quarter for incident cases) to the end of the first follow-up year.
Study design (a) and algorithms used to validate outpatient SLE diagnoses (b). aSLE codes (M32.1, M32.8, M32.9) AND outpatient diagnosis by a specialist. bANA + anti-dsDNA or ANA + other ENAs or ANA + Cardiolipin Ab or ANA + lupus anticoagulant or ANA + > 1 C3 or C4. cICD-10 codes (N08.5, N16.4, J99.1, I32.8, I39.x, D59.1, K75.4, G63.5, G05.8, and G40.x). dNo moderate/severe disease claims. eMethotrexate, azathioprine, mycophenolate mofetil, cyclosporine, belimumab, rituximab, tacrolimus, or corticosteroids (10–40 mg/day). fCyclophosphamide or corticosteroids (> 40 mg/day oral, ≥ 100 mg/day injection) or procedures: hemodialysis, peritoneal dialysis, hemodiafiltration, kidney transplantation, plasmapheresis, or immunoadsorption. Ab antibody, ICD-10 International Classification of Diseases, 10th Revision, Q quarter
An inpatient SLE episode with relevant ICD-10 primary and secondary diagnosis codes was sufficient to assign a valid SLE diagnosis. To reduce misclassification related to outpatient diagnoses, we required an outpatient SLE diagnoses in at least two quarters within 3 years, follow-back or follow-up, from the first quarter in the corresponding year, a modified version of the “at least two quarters criterion” that considers the time course of the disease [12]. Validation of an outpatient SLE diagnosis was developed with guidance from a medical expert and required an outpatient SLE diagnosis coded by a rheumatologist, nephrologist, internist, dermatologist, neurologist, pulmonologist, or gynecologist/obstetrician; supportive laboratory tests; prescriptions for anti-malarials (hydroxychloroquine, chloroquine) or immunosuppressive medications (azathioprine, methotrexate, mycophenolate or mycophenolic acid, belimumab, rituximab, cyclophosphamide, cyclosporine A, tacrolimus, systemic corticosteroids); or organ involvement (Fig. 1b). Patients with a validated outpatient or a primary hospital diagnosis of SLE in 2009 were followed through 2014.
SLE Incidence and Prevalence
Data from 2009 to 2014 were used to identify the annual number of incident and prevalent SLE cases in the BKK sample (Fig. 1a). Incident cases were defined as patients with a new SLE diagnosis in the reference year between 2009 and 2014. Prevalent cases were defined as patients with at least one SLE diagnosis between 2009 and 2014 and at least one other SLE diagnosis within the 3 years prior. To estimate SLE incidence and prevalence in the GKV population, SLE rates in the BKK sample were calculated for each 5-year age stratum by sex and applied to age- and sex-matched strata within the GKV population in the corresponding year. The sum of patients in all age strata yielded the estimate of persons with SLE in the GKV population. Patients diagnosed with SLE in outpatient care from 2012 to 2014 had fewer than the 3 years of follow-up required to confirm an SLE diagnosis because the study ended on December 31, 2014. To account for right-censored data, which may underestimate 2014 incidence and prevalence estimates, average age- and sex-adjusted probabilities were calculated for outpatients with confirmed first diagnoses in index years 2009–2011 and were applied to correct incidence and prevalence estimates for patients diagnosed in 2014.
SLE Severity–Related Algorithm
To assign SLE severity at baseline, otherwise not identifiable in health insurance databases, we developed an algorithm based on clinical practice in Germany by screening for specific ICD-10- German Modification (GM) codes as a proxy of ‘organ involvement’, treatment and procedures, and expert estimation of severity of ICD-10-GM codes (Supplementary Table S1; Fig. 1b). SLE was classified as severe if a patient received either cyclophosphamide or high-dosage corticosteroids (> 40 mg/day orally or daily injection ≥ 100 mg), or if a patient was undergoing hemodialysis, peritoneal dialysis, hemodiafiltration, kidney transplantation, plasmapheresis, or immunoadsorption. Moderate SLE was defined by no cyclophosphamide or high-dosage corticosteroids, but treatment with methotrexate, azathioprine, mycophenolate mofetil, cyclosporine, belimumab, rituximab, tacrolimus, or corticosteroid dosage 10–40 mg/day. If these criteria for severe or moderate SLE were not met, patients were considered to have mild SLE.
Longitudinal Trends in SLE Healthcare Resource Utilization and Costs
Healthcare resource utilization and costs over time were analyzed for all patients with a primary hospital diagnosis and/or a validated outpatient diagnosis of SLE in 2009. Resource utilization measures included annual outpatient/ambulatory treatment (number of visits, diagnosis), inpatient treatment/hospitalizations (number of hospitalizations, mean duration of hospitalizations, diagnosis), and prescription use (corticosteroids, anti-malarials, non-steroidal anti-inflammatory drugs, immunosuppressants, biologics, or other medications). Cost measures included annualized inpatient and outpatient/ambulatory treatment costs and other benefits (including transport, home nursing care, rehabilitation, physiotherapy, acupuncture, homeopathic therapy) and prescription costs. Cost of sickness benefits paid and average number of days of work disability were also measured.
Cost and utilization outcomes of patients with SLE identified in 2009 were compared with age-, sex-, and Charlson Comorbidity Index (CCI)–matched controls. Individuals in the control population had to be completely insured throughout the study and could not have an M32 ICD-10 diagnosis code for SLE between 2006 and 2014. Baseline CCI was assigned in the SLE and control populations based on patient characteristics in 2009 and used to stratify the population. Matched controls (1:4) were randomly assigned from corresponding age-sex-CCI stratum.
Statistical Analysis
Categorical variable distributions were described by number and proportion of patients. Continuous variables were summarized by mean, standard deviation (SD), median, and range of values. Mean costs were compared across SLE and control samples by SLE disease severity.
Continuous outcomes were compared using the non-parametric Wilcoxon–Mann–Whitney test [13]. Bonferroni corrections were performed for multiple comparisons. Data were analyzed using SAS BASE and SAS STAT software version 9.4 (Cary, NC, USA).
Results
Baseline Characteristics
In 2009, 1228 patients with SLE were identified and 1177 patients had a confirmed SLE diagnosis after validation of outpatient diagnoses. After 17 patients were excluded (reasons being not completely insured during the index quarter [n = 3], < 18 years of age [n = 14]), 1160 patients were included in this analysis (Fig. 1b).
Most of these patients were female (84.1%), with mean age of 51.2–51.9 years (SD 16.6 years) across study years. Age within the entire BKK sample was representative of the GKV population in 2009 (Supplementary Figure S1). Sex distribution was also comparable, with women accounting for 49% of the BKK sample and 53% of the GKV population. Serious SLE-related organ involvement was present in 22.5% (261/1160) of patients, of whom 46.0% (n = 120) had lupus nephritis, 32.2% (n = 84) had epilepsy, and 9.6% (n = 25) had hemolytic anemia at baseline.
The SLE severity algorithm at baseline identified 148 (12.8%) patients with mild, 484 (41.7%) moderate, and 528 (45.5%) severe SLE (Fig. 1b). The most common disease manifestations at baseline were mucocutaneous (78.7%; n = 913), osteoarticular (38.5%; n = 446), neuropsychiatric/neurological (24.1%; n = 280), vascular (22.3%; n = 259), renal (22.0%; n = 255), and immunological (20.2%; n = 234; Table 1). Organ involvement, being osteoarticular, neuropsychiatric/neurological, renal, immunological, respiratory, ophthalmologic, and hematologic, was more common with moderate or severe SLE than mild SLE (Table 1).
Incidence and Prevalence of SLE in Germany
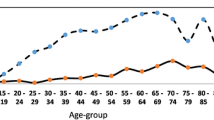
SLE incidence within the BKK population was 5.96 per 100,000 persons in 2009, with an increasing trend from 2010 to 2012 and a mild decline in 2013 and 2014 (Table 2). The 2014 adjusted incidence of SLE in the German population was 8.82 per 100,000. The corresponding SLE prevalence was 37.32 per 100,000 persons in 2009, increasing to 47.36 per 100,000 persons in 2014. The adjusted SLE prevalence in Germany was 55.80 per 100,000 persons (Table 2).
After age- and sex-adjusted extrapolation to the GKV population, the estimated SLE incidence followed similar trends as for the BKK population, with higher incidence in female patients. In 2009, estimated SLE incidence was 6.1 (male, 1.91; female, 9.79) per 100,000 persons, contrasting with an overall incidence of 4.66 (male, 1.96; female, 7.10) in 2014. Within the German population, the estimated SLE prevalence ranged from 38.61 (male, 11.62; female, 62.56) per 100,000 persons in 2009 to 48.50 (male, 13.78; female, 79.78) in 2014. When corrected for right censoring, SLE incidence was highest in 2014: corrected SLE incidence 8.82 (male, 3.37; female, 13.72) per 100,000 persons. The corrected estimated SLE prevalence in 2014 was 55.80 (male, 16.28; female, 91.39) per 100,000 persons (Table 2).
Healthcare Utilization and Costs
In all, 1063 of 1160 patients received at least one prescription between index diagnosis and the end of the study: 83.9% received corticosteroids, 56.9% anti-malarials (hydroxychloroquine or chloroquine), 28.0% azathioprine, 15.0% mycophenolate mofetil or mycophenolic acid, 3.4% rituximab, and 2.1% belimumab (data not shown). A total of 407 of 1160 (35.1%) patients had hospitalizations during the study period with a primary diagnosis of SLE.
One year after diagnosis, mean (SD) annual all-cause healthcare costs per capita were €6895 (14,424) for patients with SLE compared with €3692 (3994) for controls, 1.87-fold higher for patients with SLE (Fig. 2a). Mean annual all-cause healthcare costs for patients with SLE were consistently higher compared with controls, and for patients with moderate or severe SLE compared with controls matched by age, sex, and CCI.
Patients with SLE utilized more healthcare resources. Each year, over the course of the follow-up period, 97.8–98.6% of patients with SLE vs. 93.4–95.6% of controls received at least one prescription (Table 3). During follow-up, 30.8–38.1% of patients with SLE were hospitalized annually compared with 18.9–21.5% of controls. The proportion of patients with SLE who received hospital care without an overnight stay increased from 6.8% (year 1) to 28.6% (year 5); the increase was less pronounced in the control group (3.5–11.1%; Table 3).
Other benefits, a heterogenous group of outpatient/ambulatory benefits, were used by 61.9–74.6% of patients with SLE vs. 53.4–67.1% in the control group (Table 3). Patients with SLE and matched controls used similar amounts of short- and long-term sick leave. SLE short- and long-term disability use over the study period ranged from 23.7 to 26.0% and 3.2–4.7%, respectively.
Healthcare Resource Utilization and Costs by SLE Severity
Mean annual all-cause costs for patients with SLE increased with baseline SLE severity (Fig. 2a). Mean annual all-cause costs incurred for patients with severe SLE exceeded those for matched controls by 2.1- to 2.5-fold across study years. Among patients with severe SLE, mean (SD) all-cause costs ranged between €8396 (15,770) and €10,001 (19,253) across the study periods and between €3739 (3391) and €4239 (4416) for matched controls. Mean annual all-cause costs for patients with moderate SLE exceeded those of matched controls by 1.44- to 1.74-fold in all study years. For patients with moderate SLE, mean annual all-cause costs ranged between €4867 (8322) and €5877 (10,747) and were €3380 (3554) for matched controls 1 year after diagnosis and remained approximately the same throughout the study (Fig. 2a). Patients with mild SLE had lower mean annual all-cause costs than matched controls 1, 2, 3, and 5 years after diagnosis.
Among patients with SLE, costs for outpatient visits, hospital stays, outpatient prescriptions, and other benefits increased with disease severity (Fig. 2b). Healthcare resource utilization and costs in all service areas, excluding long-term disability, were higher among patients with severe SLE than matched controls (Fig. 2b; Table 3). Patients with moderate SLE had significantly higher utilization and costs in all areas, excluding long- and short-term disability throughout follow-up and other benefits 4 years after diagnosis, compared with matched controls (P < 0.01). In contrast, healthcare resource utilization by patients with mild SLE and matched controls was similar in all service areas except for higher hospital care without overnight stay among patients with SLE (Table 3).
Annual costs of outpatient prescriptions were significantly higher for the severe SLE group vs. matched controls (€2115–2582 vs. €998–1100; P < 0.0001) and for the moderate SLE group vs. matched controls (€1152–1539 vs. €779–861; P < 0.0001). Patients with mild SLE had lower outpatient prescription costs than matched controls.
Patients with severe SLE had higher annual hospitalization rates (36.9–47.9%) than matched controls (20.5–24.1%) (Table 3). Hospitalization rates for patients with severe SLE were higher compared with patients with mild or moderate SLE (36.9–47.9% vs. 14.6–20.0% and 26.2–33.5%, respectively).
Costs by Incidence and Prevalence
Mean annual all-cause costs were consistently higher throughout follow-up for incident cases of SLE compared with prevalent cases (Table 4). The only exceptions were for severe SLE 2 years after diagnosis and mild SLE 4 years after diagnosis. Healthcare costs increased with increasing baseline disease severity, except 2 years after diagnosis, when patients with moderate incident SLE had higher costs. Mean annual all-cause costs for patients with severe disease ranged from €7497–14,179 for incident and €8334–9496 for prevalent SLE. Among patients with moderate SLE at baseline, mean annual all-cause costs ranged from €5887–8760 (incident SLE) and €4332–5505 (prevalent SLE); for mild SLE, costs ranged from €2215–3867 (incident SLE) and €1759–3300 (prevalent SLE; Table 4).
Discussion
SLE trends in Germany between 2009 and 2014 suggest increasing incidence of SLE, from 6.1 per 100,000 persons in 2009 to 8.82 per 100,000 in 2014. Similarly, prevalence increased from 38.61 to 55.80 per 100,000. Our findings demonstrate that patients with SLE incurred greater annual healthcare costs than matched controls in all years evaluated. The annual costs of healthcare utilization increased with SLE severity, and costs for incident SLE were higher than for prevalent SLE. All-cause SLE costs ranged from €1890–3010 for mild, €4867–5877 for moderate, and €8396–10,001 for severe SLE between 2009 and 2014. This study, the first to use health insurance fund data to examine SLE healthcare resource utilization and costs by disease severity in Germany, deepens our understanding of the SLE burden.
Although health insurance fund databases do not allow for clinical assessment of disease severity, we categorized patients as having mild, moderate, or severe SLE using a newly developed algorithm that uses ICD-10-GM codes as a proxy for organ involvement and analysis of treatment patterns to attribute disease severity to the claims data. The consistency of our findings throughout the follow-up period, including that baseline SLE severity was associated with healthcare resource utilization and costs, suggests that the burden of SLE may be reduced with early and effective treatment and supports the validity of our algorithm. The greater all-cause costs for patients with moderate or severe SLE compared with age-, sex-, and CCI-matched patients with other illness may be explained by the nature of the CCI, which was designed to predict mortality risk and not costs [14]. Despite this original intent, the CCI is a validated comorbidity index that is commonly implemented to analyze claims data [11]. In addition, patients with SLE and patients with other illnesses were matched by CCI at baseline, and the costs were assessed during the follow-up period. Patients in the two groups may not have had similar illness severities throughout the follow-up because of differences between the courses of SLE and other illnesses. Patients with mild SLE had lower mean annual all-cause and outpatient prescription costs than matched controls and may reflect manifestations of mild disease.
The use of administrative algorithms to characterize SLE severity has been previously evaluated [15, 16]. Speyer and colleagues compared the SLE disease severity classifications made using an administrative algorithm with the clinical disease activity measured using the SLE Disease Activity Index-2000 (SLEDAI-2 K) in the same patients. The administrative algorithm and the SLEDAI-2 K had moderate agreement in distinguishing between mild and moderate to severe SLE [17].
The 2019 European League Against Rheumatism (EULAR) guidelines recommend rituximab for patients with severe SLE [18] rather than for moderate SLE, as defined in our algorithm based on German guidelines and practice. This difference does not affect the overall disease severity classification in our study because during the study period, 2006–2014, only 20 (1.7%) patients with SLE received one or more rituximab prescription.
Our findings on the burden of SLE in Germany are consistent with those from other countries. In the United States, increased SLE severity is associated with higher healthcare costs [15, 19]. In a large Medicaid population [20], mean annual SLE medical costs decreased between the first and second years and then increased over the next 3 years, possibly owing to increasing frequency and severity of flares or worsening disease progression [20]. Other countries report an approximately two- to three-fold cost increase for patients with severe compared with non-severe SLE in the United States [15, 21], Canada [22], the United Kingdom [23], and Greece [24].
Earlier studies have demonstrated an association between corticosteroid use and organ damage in SLE [25, 26]. Our finding that > 90% of patients were receiving corticosteroid treatment may suggest the need for new, corticosteroid-sparing treatment options.
Previous studies have not focused on disease severity and associated healthcare costs in German patients with SLE. However, 77 German patients were included in an observational European study (Systemic Lupus Erythematosus Cost of Care In Europe, LUCIE) that evaluated healthcare resource utilization costs per national tariffs [27]. In the LUCIE study, mean annual direct SLE medical costs of patients with SLE in Germany were €3452, with costs for severe SLE being 3.4-fold higher vs. non-severe SLE (€5291 vs. €1565) [27], which is comparable to our findings.
Our overall incidence rate of 8.82 per 100,000 is higher than the incidence of 3.32 cases per 100,000 reported in France in 2010 using national administrative claims data [28]. This difference may reflect a true difference or may be the result of differences in SLE incidence definitions; code sensitivity, specificity, and accuracy; or population demographics [28]. Our incidence rates (male, 3.37; female, 13.72 per 100,000 person-years) are higher than a 2002 estimate of the SLE incidence in Germany (male, 0.9; female, 1.9 per 100,000 person-years) [29]. The increase may be owing to improved SLE diagnostics or greater exposure to risk factors [30]. We estimate that the SLE incidence in Germany increased from 6.1 per 100,000 persons in 2009 to 8.82 in 2014. Incidence has also increased in Denmark (1.1–2.5 per 100,000 person-years from 1985–1989 to 1990–1994) [31] and Greece (1.4–2.1 per 100,000 person-years from 1982−1986 to 1997–2001) [32]. These increases may be due in part to greater disease awareness among patients and physicians, improved access to health services, or better diagnostics [31, 32]. In contrast, Rees et al. reported decreases in SLE incidence during similar periods in the United Kingdom (1999−2012) and United States (1980−1992 to 1993–2005) [30]. Known differences in geographic habitation and ethnicity contribute to worldwide trends of SLE incidence [30].
The SLE prevalence in Germany of 38.61–55.80 per 100,000 from 2009 to 2014 is consistent with increasing global SLE prevalence. The prevalence in male patients (16.28 per 100,000) aligns with previous estimates for Germany (15.4 per 100,000) in 2002; however, prevalence in female patients (91.39 per 100,000) is higher than previously reported (55.4 per 100,000) [33]. Our prevalence estimate is similar to the SLE prevalence estimate of 47.0 per 100,000 reported in France in 2010, which was also calculated with data from a national administrative claims database [28].
Our study adds to the existing evidence. BKK data allowed us to identify a large SLE population that is representative of persons insured by German statutory health insurance and estimate disease measures and costs for incident and prevalent SLE. We developed a validation process to confirm SLE diagnoses and an algorithm to categorize SLE disease severity. The 5-year follow-up period allows for an evaluation of healthcare costs and resource utilization over time for patients with mild, moderate, or severe SLE at the beginning of the study.
The BKK data include up to 5.2 million insured persons in Germany and allow analysis of a spectrum of health outcome measures. BKK data have been used to study asthma [34], acute coronary syndromes treated with percutaneous coronary intervention [35], type 2 diabetes [36], advanced gastric cancer [37], and testicular cancer [38], but not SLE. Although healthcare delivery differs, trends identified in Germany may be representative across Europe because typical European medical guidelines have similarities.
Some limitations should be considered. Health insurance fund data are generated for reimbursement transactions. Therefore, assumptions were necessary to ascertain SLE diagnosis and severity. The assessment of medication use was based on prescription claims, which may not directly reflect medication adherence. It is possible that patients were prescribed medications for SLE disease states that may not align with disease severity assigned by algorithm, which may represent some misclassification of disease severity. However, the use of algorithms to assign SLE disease severity has yielded consistent findings by disease severity across several data sources and populations [15, 16, 39]. Patients may also have received drugs not captured in this database, which may suggest an underestimation of costs.
Conclusions
This evaluation of patients with SLE in Germany demonstrates a rising SLE incidence and higher healthcare resource utilization and costs compared with age-, sex-, and comorbidity-matched controls. Disease severity (moderate and severe SLE) is an important driver of healthcare resource utilization and costs. The rising SLE incidence and prevalence in Germany raise the importance of earlier diagnosis and effective treatments that may prevent or delay disease progression and reduce the burden of SLE.
References
Lisnevskaia L, Murphy G, Isenberg D. Systemic lupus erythematosus. Lancet. 2014;384:1878–88.
Yurkovich M, Vostretsova K, Chen W, Avina-Zubieta JA. Overall and cause-specific mortality in patients with systemic lupus erythematosus: a meta-analysis of observational studies. Arthritis Care Res (Hoboken). 2014;66:608–16.
Mak A, Cheung MW, Chiew HJ, Liu Y, Ho RC. Global trend of survival and damage of systemic lupus erythematosus: meta-analysis and meta-regression of observational studies from the 1950s to 2000s. Semin Arthritis Rheum. 2012;41:830–9.
Tektonidou MG, Lewandowski LB, Hu J, Dasgupta A, Ward MM. Survival in adults and children with systemic lupus erythematosus: a systematic review and Bayesian meta-analysis of studies from 1950 to 2016. Ann Rheum Dis. 2017;76:2009–16.
D’Cruz DP, Khamashta MA, Hughes GR. Systemic lupus erythematosus. Lancet. 2007;369:587–96.
Navarra SV, Guzman RM, Gallacher AE, et al. Efficacy and safety of belimumab in patients with active systemic lupus erythematosus: a randomised, placebo-controlled, phase 3 trial. Lancet. 2011;377:721–31.
Bjork M, Dahlstrom O, Wettero J, Sjowall C. Quality of life and acquired organ damage are intimately related to activity limitations in patients with systemic lupus erythematosus. BMC Musculoskelet Disord. 2015;16:188.
Turchetti G, Yazdany J, Palla I, Yelin E, Mosca M. Systemic lupus erythematosus and the economic perspective: a systematic literature review and points to consider. Clin Exp Rheumatol. 2012;30:S116–22.
Pilny A, Wubker A, Ziebarth NR. Introducing risk adjustment and free health plan choice in employer-based health insurance: evidence from Germany. J Health Econ. 2017;56:330–51.
Busse R, Blumel M, Knieps F, Barnighausen T. Statutory health insurance in Germany: a health system shaped by 135 years of solidarity, self-governance, and competition. Lancet. 2017;390:882–97.
Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–9.
Bauhoff S, Fischer L, Gopffarth D, Wuppermann AC. Plan responses to diagnosis-based payment: Evidence from Germany’s morbidity-based risk adjustment. J Health Econ. 2017;56:397–413.
Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47:1245–51.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.
Garris C, Jhingran P, Bass D, Engel-Nitz NM, Riedel A, Dennis G. Healthcare utilization and cost of systemic lupus erythematosus in a US managed care health plan. J Med Econ. 2013;16:667–77.
Nightingale AL, Davidson JE, Molta CT, Kan HJ, McHugh NJ. Presentation of SLE in UK primary care using the Clinical Practice Research Datalink. Lupus Sci Med. 2017;4:e000172.
Speyer CB, Li D, Guan H, et al. Comparison of an administrative algorithm for SLE disease severity to clinical SLE disease activity index scores. Rheumatol Int. 2020;40:257–61.
Fanouriakis A, Kostopoulou M, Alunno A, et al. 2019 update of the EULAR recommendations for the management of systemic lupus erythematosus. Ann Rheum Dis. 2019;78:736–45.
Clarke AE, Yazdany J, Kabadi SM, et al. The economic burden of systemic lupus erythematosus in commercially- and Medicaid-insured populations in the United States. Semin Arthritis Rheum. 2020;50:759–68.
Li T, Carls GS, Panopalis P, Wang S, Gibson TB, Goetzel RZ. Long-term medical costs and resource utilization in systemic lupus erythematosus and lupus nephritis: a five-year analysis of a large Medicaid population. Arthritis Rheum. 2009;61:755–63.
Panopalis P, Yazdany J, Gillis JZ, et al. Health care costs and costs associated with changes in work productivity among persons with systemic lupus erythematosus. Arthritis Rheum. 2008;59:1788–95.
Clarke AE, Urowitz MB, Monga N, Hanly JG. Costs associated with severe and nonsevere systemic lupus erythematosus in Canada. Arthritis Care Res (Hoboken). 2015;67:431–6.
Khamashta MA, Bruce IN, Gordon C, et al. The cost of care of systemic lupus erythematosus (SLE) in the UK: annual direct costs for adult SLE patients with active autoantibody-positive disease. Lupus. 2014;23:273–83.
Bertsias G, Karampli E, Sidiropoulos P, et al. Clinical and financial burden of active lupus in Greece: a nationwide study. Lupus. 2016;25:1385–94.
Al Sawah S, Zhang X, Zhu B, et al. Effect of corticosteroid use by dose on the risk of developing organ damage over time in systemic lupus erythematosus-the Hopkins Lupus Cohort. Lupus Sci Med. 2015;2:e000066.
Bruce IN, O’Keeffe AG, Farewell V, et al. Factors associated with damage accrual in patients with systemic lupus erythematosus: results from the Systemic Lupus International Collaborating Clinics (SLICC) inception cohort. Ann Rheum Dis. 2015;74:1706–13.
Richter JG, Hackel B, Manger K, et al. What factors determine the direct medical costs of patients with systemic lupus erythematosus in Germany? Subanalysis of the LUCIE study. Gesundheitswesen. 2014;76:41–3.
Arnaud L, Fagot JP, Mathian A, Paita M, Fagot-Campagna A, Amoura Z. Prevalence and incidence of systemic lupus erythematosus in France: a 2010 nation-wide population-based study. Autoimmun Rev. 2014;13:1082–9.
Brinks R, Hoyer A, Weber S, et al. Age-specific and sex-specific incidence of systemic lupus erythematosus: an estimate from cross-sectional claims data of 2.3 million people in the German statutory health insurance 2002. Lupus Sci Med. 2016;3:e000181.
Rees F, Doherty M, Grainge MJ, Lanyon P, Zhang W. The worldwide incidence and prevalence of systemic lupus erythematosus: a systematic review of epidemiological studies. Rheumatology (Oxford). 2017;56:1945–61.
Voss A, Green A, Junker P. Systemic lupus erythematosus in Denmark: clinical and epidemiological characterization of a county-based cohort. Scand J Rheumatol. 1998;27:98–105.
Alamanos Y, Voulgari PV, Siozos C, et al. Epidemiology of systemic lupus erythematosus in northwest Greece 1982–2001. J Rheumatol. 2003;30:731–5.
Brinks R, Fischer-Betz R, Sander O, Richter JG, Chehab G, Schneider M. Age-specific prevalence of diagnosed systemic lupus erythematosus in Germany 2002 and projection to 2030. Lupus. 2014;23:1407–11.
Friedel H. Virchow JC [Health care of asthma patients in combination therapy with ICS and LABA—an analysis of statutory health insurance data]. Pneumologie. 2014;68:336–43.
Friedel H, Delges A, Clouth J, Trautvetter DT. Expenditures of the German statutory health insurance system for patients suffering from acute coronary syndrome and treated with percutaneous coronary intervention. Eur J Health Econ. 2010;11:449–55.
Sittig DT, Friedel H, Wasem J. Prevalence and treatment costs of type 2 diabetes in Germany and the effects of social and demographical differences. Eur J Health Econ. 2015;16:305–11.
Friedel H, Clouth J, Brück P, et al. A retrospective observational study of the epidemiology of advanced gastric cancer in Germany. An analysis of health insurance data from a central database. Gesundheitsökonomie und Qualitätsmanagement. 2015;20:108–13.
Rusner C, Stang A, Dieckmann KP, Friedel H. Frequency of computed tomography examinations in the follow-up care of testicular cancer patients—an evaluation of patterns of care in Germany. Onkologie. 2013;36:188–92.
Murimi-Worstell IB, Lin DH, Kan H, et al. Healthcare utilization and costs of systemic lupus erythematosus by disease severity in the United States. J Rheumatol. 2020. https://doi.org/10.3899/jrheum.191187.
Acknowledgements
Funding
This work and the journal’s Rapid Service Fee were supported by AstraZeneca (Cambridge, United Kingdom).
Medical Writing, Editorial, and Other Assistance
Medical writing assistance was provided by Ellen Stoltzfus, PhD, and Kathryn Fogarty, PhD (JK Associates, Inc., part of Fishawack Health, Conshohocken, PA, USA) and funded by AstraZeneca. The first draft of this manuscript was prepared by Bitte Kantar Health Namen und Funktionen eintragen, Maria Niki Aigyptiadou, MD, PhD, MBA.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Prior Presentation
The findings reported in the current manuscript were presented, in part, at the 2017 American College of Rheumatology and Association of Rheumatology Health Professionals (ACR/ARHP) 2017 meeting. (Hammond ER, Friedel H, Garal-Pantaler E, Pignot M, Velthuis E, Wang X, Nab H, Desta B, Schwarting A. Health Care Costs of Patients with Systemic Lupus Erythematosus (SLE) Versus Control Patients As a Function of Disease Severity: Analysis of the Betriebskrankenkassen German Sickness Fund [abstract number 195]. Arthritis Rheumatol. 2017;69(suppl 10).
Disclosures
A.S. was supported by the RARENET EU-Interreg project. H.F. and E.G.-P. have nothing to disclose. M.P. is an employee of Kantar GmbH and conducted work on behalf of AstraZeneca. X.W., B.D., and E.R.H are employees of AstraZeneca. H.N. is a former employee of AstraZeneca.
Compliance with Ethics Guidelines
Health insurance companies were informed about the project, and required approvals were obtained. Patient-level data in the database are anonymized to comply with German data protection regulations. Use of this database for health services research is fully compliant with German federal law, and accordingly, Institutional Review Board/ethical approval was not required because all patient-level data in the database are anonymized. The study conformed with the Helsinki Declaration of 1964, as revised in 2013, concerning human and animal rights. Springer’s policy concerning informed consent does not apply to this analysis of de-identified claims data.
Data Availability
The data underlying this article were provided by the BKK German Sickness Fund Database by permission. The datasets generated during and/or analyzed during the current study are not publicly available due to data privacy.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Schwarting, A., Friedel, H., Garal-Pantaler, E. et al. The Burden of Systemic Lupus Erythematosus in Germany: Incidence, Prevalence, and Healthcare Resource Utilization. Rheumatol Ther 8, 375–393 (2021). https://doi.org/10.1007/s40744-021-00277-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40744-021-00277-0